Shiga Toxin-Mediated Hemolytic-Uremic Syndrome (ST-HUS)
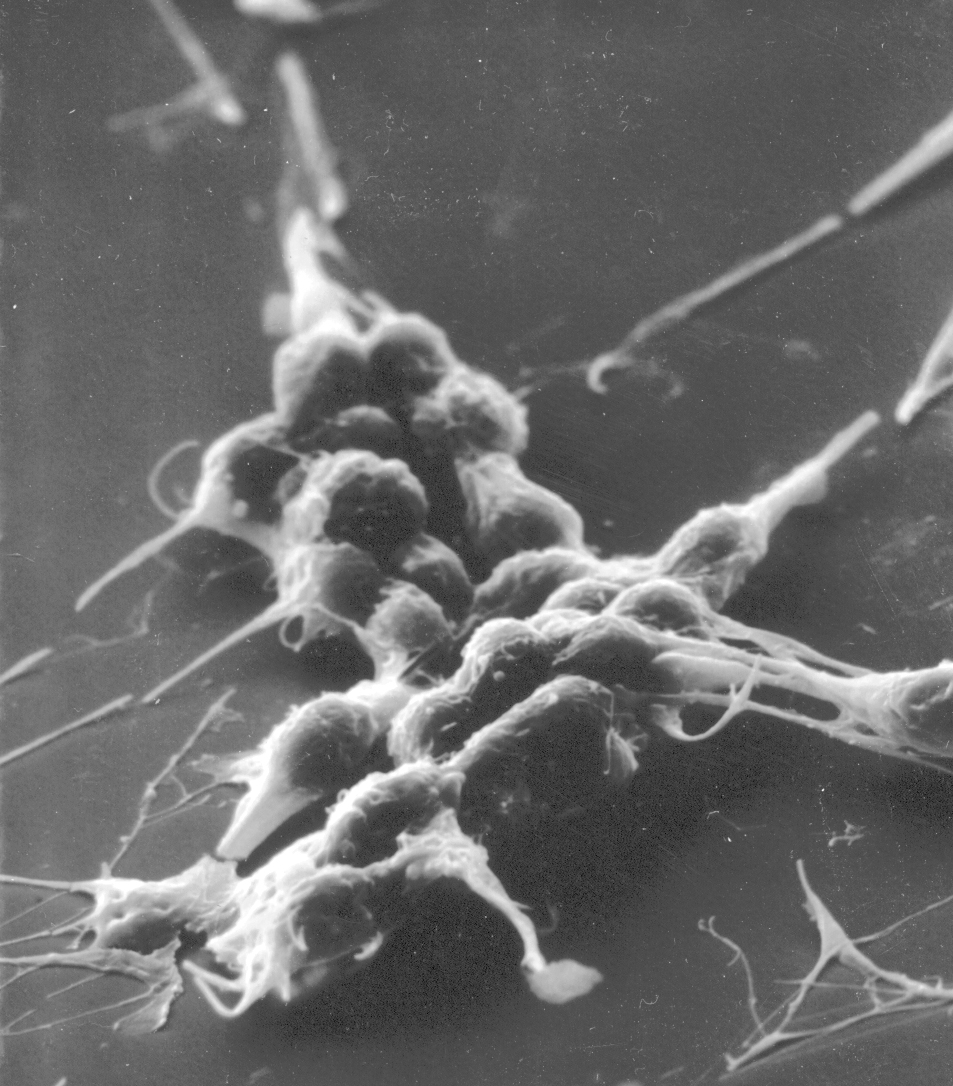
ST-HUS is caused by a toxin secreted from bacteria causing an intestinal infection. The toxin is named Shiga toxin. The bacteria which secrete Shiga toxin are Shigella dysenteriae, which causes intestinal infection with severe diarrhea most commonly in Asia, and certain strains of Escherichia coli (abbreviated as E. coli), which cause most of the ST-HUS in the Americas and Europe. The strains of E. coli that secrete Shiga toxin are designated by letters and numbers. The most common strain in the US and Europe is E. coli O157:H7. The strain that caused a severe outbreak in Germany in 2011 was E. coli O104:H4. These bacteria commonly occur in the intestinal tract of cattle, where they cause no harm. In contrast, in humans, eating only a few these E. coli can cause serious illness. As expected, exposure to these strains of E. coli can come from contact with cattle on farms, or from undercooked meat, or from uncooked vegetables that became contaminated with E. coli from cattle if, for example, the vegetable preparation was next to a cattle barn or stockyard.
Different people have different susceptibilities to these infections. For example, if a family all eats the same contaminated food, some will have severe bloody diarrhea and kidney failure (this is ST-HUS). Others will only have diarrhea. And others may not get sick at all. Typically children less than 4 years old are most susceptible.
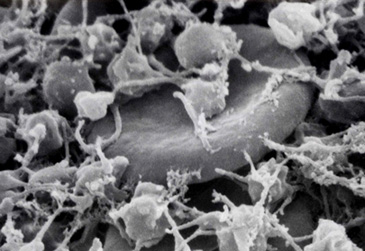
The typical course of illness in children with ST-HUS begins with diarrhea, abdominal pain, fever, and vomiting about 3 days after the exposure. Two or three days later, the diarrhea becomes overtly bloody. Then, after several more days, the diarrhea improves but the HUS begins: the platelet count and hemoglobin concentration fall and kidney failure occurs. The kidney failure can be severe and require dialysis, but it almost always resolves. There is no specific treatment. Plasma exchange, as used for TTP, is not known to be effective although it is used in some patients with critical illness.
Publications:
1. This article describes the causes and clinical course of children with ST-HUS.
Tarr PI, Gordon CA, Chandler WI. Shiga toxin-producing Escherichia coli and hemolytic uremic syndrome. Lancet 2005; 365: 1073-1086. [Full Text]
2. This article describes the clinical features of children with ST-HUS and contrasts these features with adults who get ST-HUS.
Karpac CA, Li X, Terrell DR, Kremer Hovinga JA, Lämmle B, Vesely SK, George JN. Sporadic bloody diarrhoea-associated thrombotic thrombocytopenic purpura-haemolytic uraemic syndrome: an adult and paediatric comparison. British J Haematol 141: 696-707, 2008. [Full Text]
3. This article describes the experience with ST-HUS in Oklahoma, 2002-2005, a rural state with extensive cattle farms. Almost all patients infected by E. coli O157:H7 were single individuals, with no identification of the source of the infection. This study documents that these infections are endemic and almost always sporadic – not associated with identified outbreaks.
Karpac CA, Lee A, Kunnel BS, Bamgbola OF, Vesely SK, George JN. Endemic Escherichia coli O157:H7 infections and hemolytic-uremic syndrome in Oklahoma, 2002-2005, Journal of the Oklahoma State Medical Association 100: 429-433, 2007.
4. These 3 articles describe large outbreaks of ST-HUS, and how they occur.
The outbreak in Seattle in 1993 was the first well described outbreak of by E. coli O157:H7 infection. It came from undercooked hamburgers from a specific fast-food chain of restaurants. 501 cases of diarrhea occurred; 45 people developed HUS; 3 people died.
Bell BP, et al. A multistate outbreak of Escherichia coli O157:H7-associated bloody diarrhea and hemolytic uremic syndrome from hamburgers. JAMA 1994; 272 (17): 1349-1353. [Link to article]
The outbreak in Germany in 2011 was caused by E. coli O104:H4 in raw sprouts from one source which presumably became contaminated from soil containing cattle manure. 3816 cases of diarrhea occurred; 845 people developed HUS; 54 people died.
Frank C, et al. Epidemic profile of Shiga toxin-producing Escherichia coli O104:H4 outbreak in Germany. New Eng J Med 2011; 365 (19): 1771-1780. [Full Text]
This article describes an outbreak in 26 states of the US in 2006 related to fresh spinach from a single producer. 199 cases of diarrhea occurred; 31 people developed HUS; 3 people died. This article tells the story of how these outbreaks happen.
Maki DG. Don’t eat the spinach – controlling foodborne infectious disease. New Eng J Med 2006; 355 (19): 1952-1955. [Full Text]
James N. George, M.D.
Professor of Medicine
Hematology-Oncology Section, Department of Medicine
Department of Biostatistics & Epidemiology, College of Public Health
University of Oklahoma Health Sciences Center
IMPORTANT!
The information included in this website is for educational purposes only. The designers and operators of this site take no responsibility for the things you may do with this information. For advice on your unique medical condition, please consult your health care professional. By going further into this website you acknowledge that you have read and understood this disclaimer.