Complement-Mediated Thrombotic Microangiopathy (C-TMA)
Complement-mediated TMA, abbreviated as C-TMA, is caused by abnormalities of regulation of the alternative pathway of complement activation. The complement system of plasma proteins is part of our immune system. These are not like antibodies, which are produced by an immune response to a specific infectious agent (such as bacteria) or other foreign substances (such as a transplanted kidney). The complement system is like a general surveillance system, which helps to fight infection but is also responsible for cleaning up injured tissues. The system of complement proteins is only minimally active unless an infection or tissue injury is present. Then the system activates and generates the proteins that can help to kill infectious agents (such as bacteria) or to clean up injured tissues and begin the healing process.
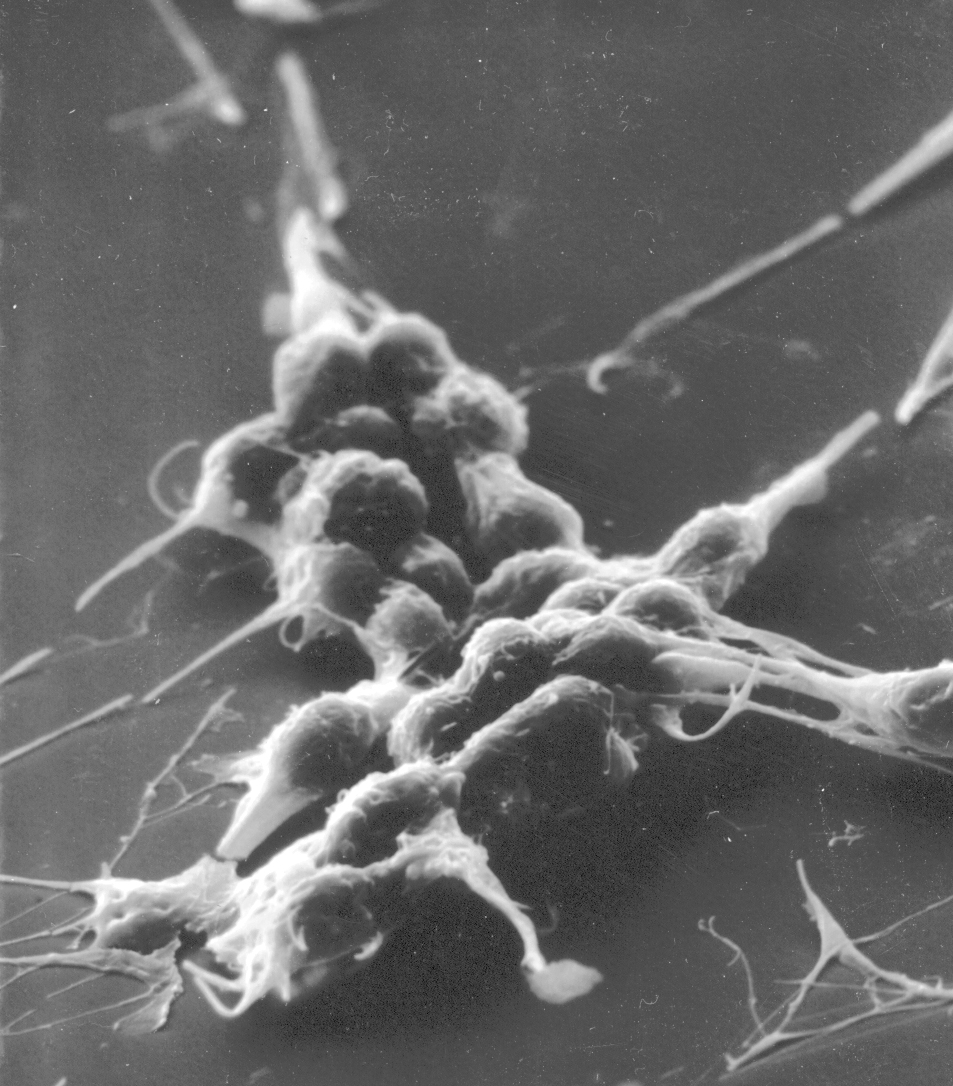
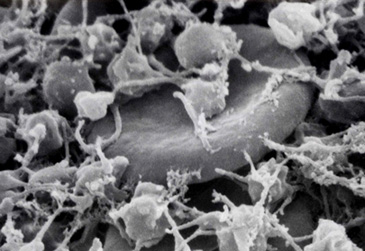
In patients with C-TMA, the regulation of complement activation does not function properly and complement proteins become activated inappropriately. This results in damage to normal tissues. The inappropriately activated complement proteins can cause severe kidney damage – as well as the other features of TMA, such as a low platelet count and damage of red blood cells.
The cause of C-TMA is thought to be a genetic abnormality. Proteins that normally restrict complement activation are not effective or those that normally accelerate complement activation are too effective. A specific anti-complement treatment (eculizumab; its brand name is Soliris) can block the inappropriate activation of complement. However a problem with the diagnosis of C-TMA is that the genetic analysis to identify the abnormalities that are associated with C-TMA is complex and the results are not available when a diagnosis needs to be made and treatment given.
Our understanding of C-TMA is not complete. Many patients who seem to have C-TMA do not have the genetic mutations that affect complement activation. Also people can have the genetic mutations that affect complement activation and never have any signs of C-TMA during their lifetime. Certain conditions, such as pregnancy, can trigger the occurrence in susceptible people.
Therefore these three critical questions about C-TMA often cannot be answered with confidence.
- Which patients with signs of a TMA syndrome need treatment with eculizumab?
- If eculizumab is started, how long does it need to be continued?
- When a patient recovers from C-TMA, what is the risk for relapse?
Publication:
Loriat C, et al. An international consensus approach to the management of atypical hemolytic syndrome in children. Pediatric Nephrology 2015; published on line 11 April 2015. [Full Text]
This publication summarizes our current knowledge about C-TMA (which the authors named “atypical HUS”). It describes diagnosis and treatment. Although the focus is on children, the principles are the same for adults.
James N. George, M.D.
Professor of Medicine
Hematology-Oncology Section, Department of Medicine
Department of Biostatistics & Epidemiology, College of Public Health
University of Oklahoma Health Sciences Center
IMPORTANT!
The information included in this website is for educational purposes only. The designers and operators of this site take no responsibility for the things you may do with this information. For advice on your unique medical condition, please consult your health care professional. By going further into this website you acknowledge that you have read and understood this disclaimer.