Biomechanics of the hand
Gwenda Sharp OTR and Dave Thompson PT
Some biologists believe that the development of the human hand accorded an advantage to the development of a large and complex brain.
The hand's very existence potentiated brain development by allowing humans to manipulate, interact with, explore, and gain information from their environment.
Development of a more complex brain permitted us in turn to make and use tools and to develop language, which in turn led to the growth of an elaborate system of shared meanings, what we know as culture.
Two types of grasp are differentiated (Smith, Weiss, & Lehmkuhl, 1995, pp. 216-219; Hertling & Kessler, 1996, pp.259-260) according to the position and mobility of the thumb's CMC and MP joints.
- POWER grasp (The terms grasp, grip, and prehension are interchangeable.)
(The adductor pollicis stabilizes an object against the palm; the hand's position is static.)
- cylindrical grip (fist grasp is a small diameter cylindrical grasp)
- spherical grip
- hook grip (MP extended with flattening of transverse arch; the person may or may include the thumb in this grasp)
- lateral prehension (this can be a power grip if the thumb is adducted, a precision grip if the thumb is abducted).
- PRECISION
(Muscles are active that abduct or oppose the thumb; the hand's position is dynamic.)
- palmar prehension (pulp to pulp), includes 'chuck' or tripod grips
- tip-to-tip (with FDP active to maintain DIP flex)
- lateral prehension (pad-to-side; key grip)
Three arches balance stability and mobility in the hand.
The proximal transverse arch is rigid, but the other two arches are flexible, and are maintained by activity in the hand's intrinsic muscles.
| |
|---|
- PROXIMAL TRANSVERSE ARCH
Hertling and Kessler (p. 257) describe this arch as a composite of two arches, the proximal and distal carpal arches.)
- a stable bony arch that forms the posterior border of the carpal tunnel.
- The arch's integrity is maintained by a soft tissue "strut" formed by the flexor retinaculum or transverse carpal ligament (also called the volar carpal ligament). This ligamentous strut connects the scaphoid and trapezium on the arch's radial side with the hamate on its ulnar side, and forms the anterior border of the carpal tunnel.
- DISTAL TRANSVERSE ARCH
Hertling and Kessler (p. 257) call this the metacarpal arch, because it is formed by the metacarpal heads; metacarpals 2 and 3 are stable while 4 and 5 are relatively mobile. You can observe the arch's combination of "radial" stability and "ulnar" mobility by loosely closing your fist, then squeezing more tightly, when you will observe movement in the more mobile fourth and fifth metacarpals.
- LONGITUDINAL ARCH
Observe this arch's behavior as you loosely close your fist. Tighten the fist and watch the fourth and fifth metacarpals.
The arches provide a balance between stability and mobility for grasping. For instance, we produce the so-called "chuck grasp" by using the more stable second and third metacarpals, instead of the more mobile fourth and fifth metacarpals.
Therapeutic splints must support these three arches.
Functional position of the hand
(Norkin & Levangie, 1992, p. 296; Hertling & Kessler, 1996, p. 260)
- Wrist
- extended 20 degrees
- ulnarly deviated 10 degrees
- Digits 2 through 5
- MP joints flexed 45degrees
- PIP joints flexed 30-45 degrees
- DIP joints flexed 10-20 degrees
- Thumb
- first CMC joint partially abducted and opposed
- MP joint flexed 10 degrees
- IP joint flexed 5 degrees
| Compare this figure with the one in Hertling and Kessler (1996, Fig.11-25).
|
|---|
|
|---|
When therapists immobilize a patient's hand, they often position it this way. During a period of immobilization, the resting lengths of the hand's ligaments and muscles change. This hand position provides the best balance of resting length and force production so the hand can function when the patient mobilizes it again.
Joints of the hand
| JOINT | STRUCTURE | AXIS | MOTION | CLOSE-PACKED POSITION
|
|---|
Metacarpo-phalangeal (MP)biaxial
(condylar)
lateral
A-Pflexion/extension
abduction/adduction first: extension
2nd-5th: flexion
Proximal Interphalangeal (PIP)uniaxial lateral flexion/extensionextension
Distal Interphalangeal (DIP)uniaxial lateral flexion/extensionextension
| | | | | | | | | | | | | | |
- Metacarpophalangeal (MP)
- condyloid, biaxial joints
- joint's palmar aspect is palpable at level of distal palmar crease
- proximal joint surface is convex and distal surface is concave
roll and glide occur in same direction
- anterior with flexion
- posterior with extension.
- large metacarpal joint surface
- a fibrocartilaginous volar plate is lined with hyaline cartilage so that it augments or enlarges the proximal phalanx' relatively small articular surface.
- superficial to volar plate is the transverse metacarpal ligament
- joint capsule supported by two collateral ligaments
- close-packed position:
- MP joints of digits 2 through 5: close-packed in flexion; you cannot abduct or adduct these joints when they are flexed.
- MP joint of thumb: close-packed in extension
- Interphalangeal (IP)
- uniaxial hinge joints
- supported by two collateral ligaments, and by smaller versions of a volar plate.
- Like MP joint, proximal joint surface is convex and distal surface is concave
roll and glide occur in same direction
- anterior with flexion
- posterior with extension
- close-packed in extension
Mechanism for finger flexion
- FDP: flexor digitorum profundus (the deeper of the two)
- FDS: flexor digitorum superficialis (the more superficial muscle)
Although the FDP is deep to the FDS over most of its course, it attaches to the skeleton more distally, because it passes through a 'split' in the FDS tendon.
Mechanism for finger extension
We can extend the PIP and DIP joints without also extending the MP joints.
But we can't extend the PIP joint without extending the DIP joint at the same time.
Flexing only the DIP joint without also flexing the PIP joint is difficult.
Full (active or passive) flexion of the PIP joint prevents active extension of the DIP joint.
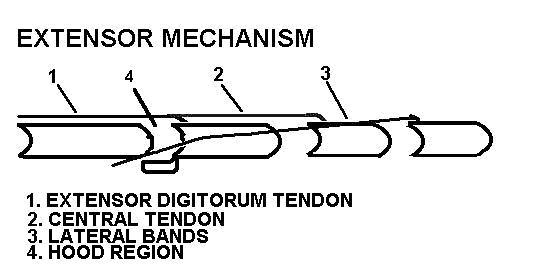
We can understand these finding by learning the structure of the EXTENSOR MECHANISM, also known as the:
- extensor expansion
- extensor assembly
- extensor apparatus
- dorsal aponeurosis
- aponeurotic sleeve
| |
The extensor mechanism is an elaboration of the extensor digitorum comunis (EDC) tendon on the dorsum of each phalanx. The extensor indicis (EI) and the extensor digiti minimi (EDM) insert into the extensor mechanisms of the second and fifth digits, respectively.
Several tendinous structures comprise the extensor mechanism:
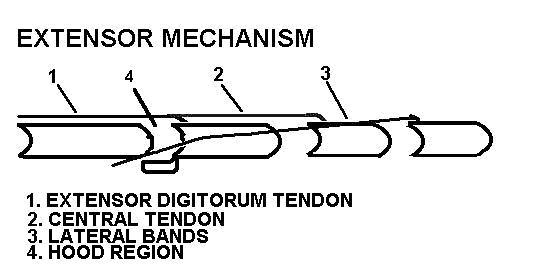
|
- The EDC tendon attaches by a tendinous slip to the proximal phalanx, through which it extends the MP joint.
- The central tendon (or "slip") proceeds dorsally to attach to base of middle phalanx, where tension can extend the PIP joint.
|
3. the lateral bands proceed on either side of dorsal midline and rejoin before attaching to the distal phalanx. Tension in the lateral bands extends the DIP joint.
4. the extensor hood surrounds the MP joint laterally, medially, and dorsally, and receives tendinous fibers from the lumbricales and interossei.
5. Fibers of the oblique retinacular ligament (ORL) attach at the sides of the proximal phalanx and digital tendon sheaths, and proceed to distal portion of lateral bands. Thus, the ORL's line of application is volar to the PIP joint's lateral axis and dorsal to the DIP joint's lateral axis.
|
PIP extension (produced by other tissues in the extensor mechanism) elongates the ORL, creating passive tension that extends the DIP. The DIP extension helps open the hand.
DIP flexion (produced by the FDP) elongates the ORL, creating passive tension that flexes the PIP. The PIP flexion assists in finger closure.
| |
|---|
| | |
More views of the extensor mechanism, adapted from Smith, Weiss, & Lehmkuhl (1996, Fig. 6-12):
Muscles that transmit force to the otherwise non-contractile extensor mechanism:
- Dorsal interossei (DI)
- Palmar interossei (PI):
- Four palmar interossei (anatomists often include the ulnar head of flexor pollicis brevis in this group) attach proximally to a metacarpal, and distally to the same digit's proximal phalanx and/or its extensor mechanism.
- They produce MP adduction and, in certain instances, MP flexion. They also produce PIP and DIP extension when they introduce tension into the extensor mechanism.
- Lumbricales:
- The four lumbricales attach proximally to the tendons of the flexor digitorum profundus, and distally to the extensor mechanism on its radial side at the level of the lateral bands. The muscles pass on the volar side of the transverse metacarpal ligament.
- If they act alone, they produce MP flexion. They also produce PIP and DIP extension when they introduce tension into the extensor mechanism.
- The lumbricales permit a dynamic interaction between flexors and extensors. Their attachments transmit their force to both the FDP tendon and the extensor mechanism. Specifically, lumbrical activity:
- increases passive tension in the extensor mechanism.
- decreases passive tension in FDP tendon's distal portion.
- Palpate the lumbricals on yourself
How does the extensor mechanism work?
Although the extensor mechanism's fibers are tendinous, and therefore incapable of producing active force, they still transmit force to their attachments.
Force develops in the extensor mechanism in two ways:
- Many of the hand's intrinsic muscles attach to the extensor mechanism. Activity in any of these muscles produces force that the extensor mechanism communicates to its distal attachments.
- The extensor mechanism develops passive tension whenever it is elongated. Hand movements that passively elongate either the extensor mechanism or a structure that attaches to the extensor mechanism produce force in the extensor mechanism itself.
The extensor mechanism's fibers have lines of application that are always dorsal to the lateral axes of the PIP and DIP joints. Therefore,
- activity in the intrinsic muscles that attach to the extensor mechanism always produces DIP and PIP extension.
- Passive flexion of the MP joint (try it yourself!) elongates the extensor mechanism and extends the PIP and DIP joints.
The fibrous lines of application in the hood and lateral bands pass very near the MP joint's lateral axis. Whether these structures move the MP joint in the sagittal plane depends on whether the MP joint is already flexed or extended.
- in MP flexion:
- MP flexion occurs when activity in the FDS or FDP flexes the MP joint.
- The extensor mechanism is not 'stretchy.' When the digits flex (at the MP, PIP, or DIP joints), passive tension in the lateral bands and central slip pull the hood distally.
- When the MP joint is already flexed, the lines of application of the interossei fall on volar side of the MP joint, and so produce MP flexion.
- The distal shift in the extensor hood also increases the lumbricales' moment arm so they can produce a greater flexor moment at the MP joint. However, your text describes EMG studies which show quite consistently that the lumbricales do not act at the same time as the FDP! The lumbricales' function evidently does not include closure of the hand.
- in MP extension:
-
Action in the extensor digitorum extends the MP joint, and also pulls the extensor mechanism (including the hood) proximally.
- In this position, the interosseous muscles' lines of application are very close to the MP joint's lateral axis.
- With such small moment arms, these muscles have little effect on MP joint movement in the sagittal plane. However, they still produce MP abduction/adduction when the MP joint is extended.
CLINICAL APPEARANCE OF PERIPHERAL NERVE INJURIES IN THE HAND
- Median:
- Often due to carpal tunnel sd.
- Wasting of thenar eminence
- Decreased thumb function, especially opposition.
- Thumb moves into plane of palm.
- Ulnar:
- Damage to ulnar nerve can occur with trauma to elbow region. Ulnar neuropathy is a frequent complication of diabetes mellitus
- Wasting of web space and interosseous spaces.
- Affects strength of intrinsic muscles of hand, so person can't hold a piece of paper between extended but adducted fingers
- Affects adductor pollicis and ulnar head of FPB. A person who lacks strength in these muscles cannot grasp with the thumb unless he or she flexes the IP joint by substituting with the flexor pollicis longus.
- Radial:
- Associated with gunshot or stab wounds, fracture of humerus, "Saturday night palsy."
- person demonstrates a "dropped wrist," and cannot reposition thumb.
- lack of wrist extension may cause hand grip to be weak.
References:
Hertling, D., & Kessler, R. M. (1996). Management of common
musculoskeletal disorders: Physical therapy principles and methods. (3rd ed.).Philadelphia: J.B. Lippincott.
Norkin, C.C., & Levangie, P.K. (1992). Joint structure and function. (2nd ed.). Philadelphia: F.A. Davis.
Smith, L.K., Weiss, E.L. & Lehmkuhl, L.D. (1996). Brunnstrom's clinical kinesiology. (5th ed.). Philadelphia: F.A. Davis.
Last updated 11-27-01 ©Dave Thompson PT
return to Control of Human Movement 1 and 2, lecture schedule